Preserving Prosperity By Extending Health Span Of Society One Patient At A Time

Nee Soon Clinic
27 Aug 2025
Traditional therapies include mouth guards, physiotherapy, and medications, but some patients are now considering Botulinum Toxin for TMJ as an alternative.
Temporomandibular joint disorder (TMJ disorder, often called TMD) is a condition that affects the hinge connecting your jawbone to your skull. It can cause chronic jaw pain, headaches, muscle stiffness, and difficulty with chewing or talking. Traditional therapies include mouth guards, physiotherapy, and medications, but some patients are now considering Botulinum Toxin for TMJ as an alternative.
This article will provide a medically accurate, comprehensive guide to Botulinum Toxin treatment for TMJ pain, what to expect, benefits, risks, and who may be an ideal candidate.
Understanding TMJ Disorder and Why Botulinum Toxin for TMJ Is Considered
What is TMJ Disorder?
The temporomandibular joint acts like a sliding hinge. Problems arise when the joint or the surrounding muscles become dysfunctional. Causes include:
Teeth grinding (bruxism)
Jaw clenching (often stress-related)
Arthritis in the joint
Injury to the jaw
Symptoms of TMJ Disorder
Common signs include:
Jaw pain or tenderness
Clicking or popping sounds when opening or closing the mouth
Headaches or ear pain
Difficulty chewing or talking
Muscle tightness in the jaw or temples
Why Botulinum Toxin for TMJ
Botulinum Toxin (onabotulinumtoxinA) is well-known for cosmetic wrinkle treatment. In medical contexts, it is used to treat conditions like chronic migraines, cervical dystonia, and hyperhidrosis. More recently, Botulinum Toxin for TMJ has been studied because:
It relaxes overactive jaw muscles.
Reduces clenching and teeth grinding.
May alleviate associated headaches and jaw tension.
How Does Botulinum Toxin for TMJ Work?
Mechanism of Action
Botulinum Toxin blocks the release of acetylcholine, a neurotransmitter that causes muscles to contract.
When injected into the masseter or temporalis muscles, Botulinum Toxin weakens overactive jaw muscles.
This leads to less clenching, reduced grinding, and improved muscle relaxation.
Treatment Process
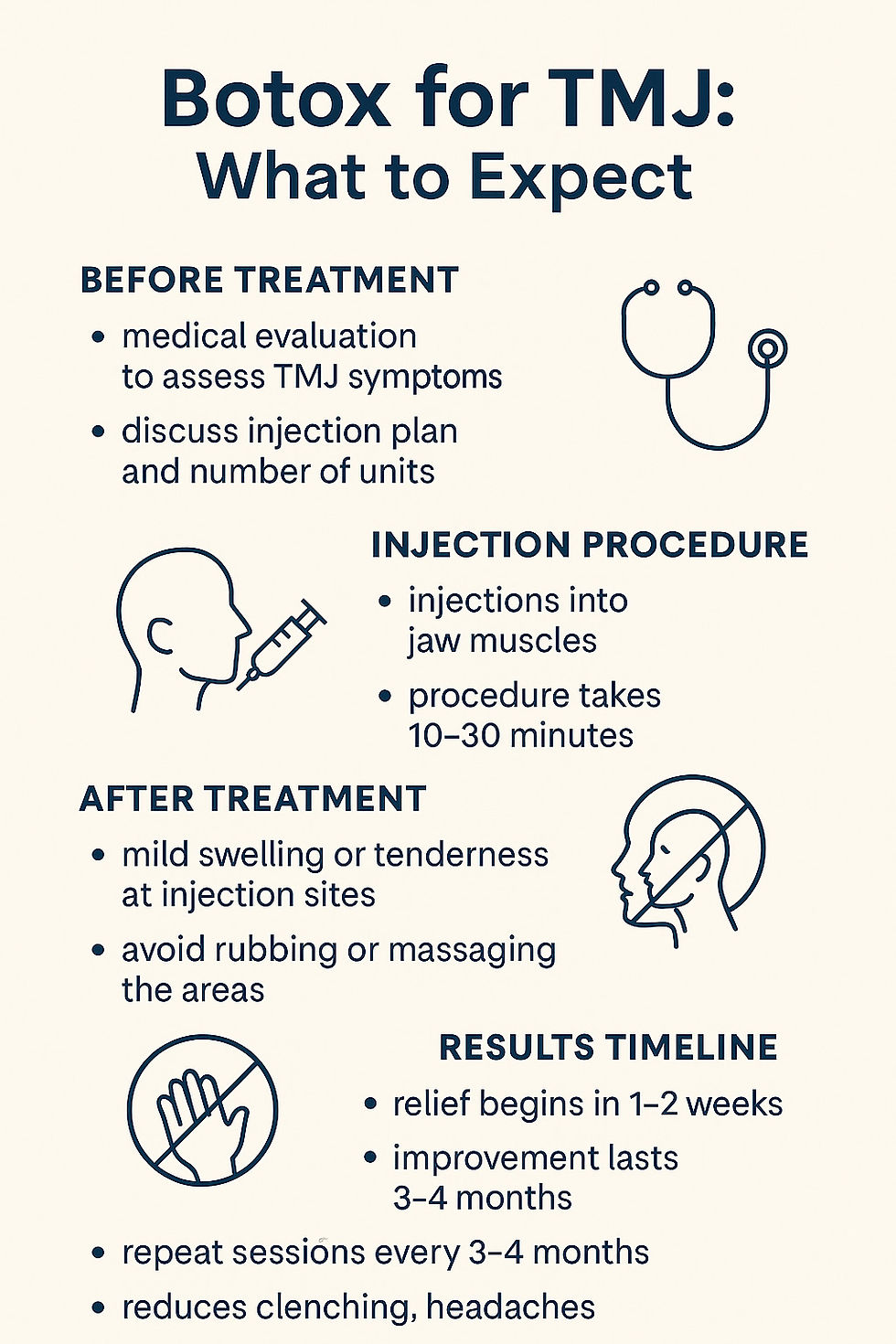
Consultation – A doctor evaluates your TMJ symptoms and medical history.
Injection – Botulinum Toxin is injected into the masseter and possibly the temporalis or pterygoid muscles.
Duration – Sessions take about 15–30 minutes.
Onset – Relief usually begins within 1–2 weeks, with full results by 4 weeks.
Maintenance – Effects last about 3–4 months; repeat treatments are recommended.
What to Expect Before and After Botulinum Toxin for TMJ
Before Treatment
Medical evaluation to rule out other causes of jaw pain.
Stop blood-thinning medications (unless prescribed) to reduce bruising.
Treatment planning: number of units and muscles targeted.
After Treatment
Mild soreness or bruising at injection sites is common.
Avoid massaging the area or lying flat for 4 hours post-injection.
Pain relief and muscle relaxation build gradually over days to weeks.
Most patients report reduced clenching, headaches, and improved jaw mobility.
Table: Timeline of Botulinum Toxin for TMJ
Stage | What Happens | Timeframe |
Immediately after | Mild swelling, possible tenderness | 0–2 days |
Early relief | Reduced muscle tension begins | 1–2 weeks |
Peak effect | Significant symptom improvement | 4 weeks |
Duration | Effects last 3–4 months | Up to 16 wks |
Repeat sessions | Needed to maintain results | Every 3–4 mo |
Benefits of Botulinum Toxin for TMJ
Pain Reduction: Decreased jaw pain and tension headaches.
Improved Function: Easier chewing, speaking, and mouth opening.
Less Teeth Grinding: Reduction in bruxism can also protect teeth.
Non-Surgical: Minimally invasive compared to surgery.
Quick Recovery: No downtime; return to normal activities immediately.
Risks and Side Effects
Although generally well-tolerated, potential risks include:
Local swelling, redness, or bruising
Temporary muscle weakness (chewing may feel different)
Rare: asymmetry of smile or difficulty chewing tough foods
Extremely rare: spread of toxin beyond injection site (FDA warnings apply)
Clinical studies have shown that most side effects are mild and resolve spontaneously. Always ensure injections are performed by a licensed medical professional.
Who Is a Candidate for Botulinum Toxin for TMJ?
Botulinum Toxin may be considered if:
You have chronic TMJ pain not relieved by standard treatments.
You grind or clench teeth excessively (bruxism).
You suffer from headaches linked to jaw muscle overuse.
You want a minimally invasive option before surgical procedures.
Contraindications include:
Pregnancy or breastfeeding
Neuromuscular disorders (e.g., myasthenia gravis)
Allergy to botulinum toxin
Alternatives to Botulinum Toxin for TMJ
Treatment | Pros | Cons |
Night guards (mouth splints) | Protects teeth, non-invasive | Does not relax muscles |
Physiotherapy | Strengthens muscles, improves mobility | Time-intensive |
Medications (NSAIDs, muscle relaxants) | Reduce inflammation/pain | Temporary, systemic side effects |
Surgery | Permanent correction in severe cases | Invasive, long recovery |
Botulinum Toxin for TMJ | Direct muscle relaxation, quick results | Needs repeat injections |
FAQs: Botulinum Toxin for TMJ
1. How many units of Botulinum Toxin are used for TMJ?
Typically 25–50 units per side, depending on muscle size.
2. How long do results last?
Most patients get relief for 3–4 months.
3. Does Botulinum Toxin for TMJ affect chewing?
Some report mild chewing fatigue early on, but this usually resolves as muscles adjust.
4. Is Botulinum Toxin FDA-approved for TMJ?
Botulinum Toxin is FDA-approved for migraines and other conditions, but use for TMJ is off-label. However, studies show it can be safe and effective when performed by trained clinicians.
5. Can Botulinum Toxin for TMJ change face shape?
Repeated injections into the masseter may slim the jawline over time, which some patients see as an aesthetic bonus.
Lifestyle Tips to Support TMJ Treatment
Even with Botulinum Toxin, lifestyle management improves results:
Reduce stress with mindfulness or yoga.
Avoid chewing gum or very hard foods.
Use warm compresses for muscle relaxation.
Practice jaw stretching exercises.
For patients in Singapore, you can learn more and book a consultation at Neesoon Clinic’s Botulinum Toxin Singapore page.
For authoritative details on Botulinum Toxin, including safety, indications, and full prescribing information, visit this information site official website.
Conclusion
Botulinum Toxin for TMJ provides a promising solution for patients with chronic jaw pain, clenching, and associated headaches. While not a cure, it can significantly reduce symptoms, improve quality of life, and protect against long-term dental damage.
Patients should consult a licensed healthcare provider to determine if this treatment is suitable. With repeat sessions and proper care, Botulinum Toxin may offer long-term relief for TMJ pain without the need for invasive surgery.
Disclaimer:
The information provided in this article is for informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. The content is not intended to be a comprehensive source of information and should not be relied upon as such. Reliance on any information provided in this article is solely at your own risk. The authors and the publisher do not endorse or recommend any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned in the article. Any reliance on the information in this article is solely at the reader's own risk.
779 Yishun Ave 2, #01-1547, Singapore 760779
Tel: 6721 9796

